Over 21,000 New Zealanders have a form of Inflammatory bowel disease (IBD) and the number is growing. Ulcerative Colitis and Crohn's disease are the biggest culprits and can often mimic the same symptoms of bowel cancer with some reports suggesting up to 15% of IBD patients go on to develop bowel cancer later in life.
Both Crohn’s Disease and Ulcerative Colitis are believed to be autoimmune diseases, where the body reacts against its own tissues.
The main difference between the two conditions is that Crohn’s Disease can affect any part of the digestive tract, Ulcerative Colitis affects only the large bowel and the rectum.
While Crohn’s Disease can affect all layers of the bowel wall, Ulcerative Colitis only affects the lining of the colon.
In severe cases, where medication and supportive treatment have not been successful in controlling the conditions, or where the side effects of medications are intolerable, surgery may be required.
Surgery may also be recommended if a growth has been found or to avoid colon cancer risk in patients who have experienced Colitis for 8 years or more or who have had severe damage to their colon.
We spoke to 37-year-old Tim Doherty from Wellington, who has recently undergone a number of bowel surgeries. This is his story...
Pre diagnosis
I haven't always been "normal" but I'm guessing most of this might have just been IBD type symptoms when there were stressful times. When I studied, at exam times especially, I noticed my bowel would work overtime, but then in the days and weeks, after the stress passed, it returned to normal. One exception was my final year of university. I had a lot of stress and in those final days, I sometimes was going to the toilet every 20 minutes!
My possible trigger to IBD
In late 2009 I needed to have my last three wisdom teeth removed, that procedure went well and as follow up I was prescribed antibiotics, anti-inflammatories and antiseptics.
I wasn't feeling too hungry at this time, but thought I had better keep up the pills! Taking these on an empty stomach brought on violent diarrhoea, However unlike the past, with time this didn't mend itself. I sought help from my GP over the next weeks and months.
During this time he checked and ruled out all the common suspects, ie food poisoning. Finally, he suggested and referred me to the gastro department of the hospital for a top and tail scope. Naturally, this wasn't something I wanted, however, with what I'd been through, I was ready for it. The GP described it as the gold standard to look for what might be wrong.
Two other things helped spot something was off. I tried to donate blood for the first time ever thinking I'll do a good deed, however, I was turned away! My count was around 90 or so and the cut off was 130. I was anaemic! I can't remember exactly but was probably losing blood in my bowel motion at the time. I was sent to get iron and talk to my GP.
At this same time, I noticed my health decline. I had decided to walk the Tongariro Crossing and while on the flat and downhill sections I was fine, however on the uphill sections my heart raced, I was breathing heavy and those around me noticed me struggling.
Diagnosis
In May 2010 I had my scopes. I found the prep not as bad as some had said! My top section was fine luckily, no Crohn's. The colonoscopy found ulcers right throughout my colon. When I was recovering I was given an A4 piece of paper full of medical jargon I didn't understand. I had a diagnosis of mild to moderate ulcerative colitis.
Treatment
I was prescribed Prednisone and these large pills which I didn't really try. I used to be horrible with pills and had to train myself to take them. In the early days, I didn't take the medication as seriously as I should. This lead to two things, my disease got worse and was noticed in scope the next year, also I got a note on my medical file saying I wasn't compliant with the medication. I had to get very serious about taking it. I got myself into a routine, I set reminders in my phone to take my meds.
I had steroids to lower my immune system. Azathioprine and then Methotrexate injections. I really hated injecting myself and after 14 months and no benefit shown, I asked to switch back to azathioprine. I had Pentasa to try to help settle my colon. I also had infusions of Infliximab at the very end, and while it was helping my bowel, it trashed my immune system at the start of winter leading to hospital stays including pneumonia.
I also picked up many other conditions that may have been related to a reduced immune system. Not only did I develop whooping cough but I contracted Hand Foot & Mouth disease too. Normally only kids under 10 years old get this! The GP only picked it up after he saw another adult with it the same week after another GP misdiagnosed it.
I got to the point where I had run out of medical options apart from taking part in drug trials. So I signed up for a trial as I really did not like the idea of surgery. However after a few weeks of monitoring, before the trial was meant to start, I was told I was not going to be able to take part. I wasn't bleeding enough for them!
The journey towards surgery
The first time this was suggested to me I was constantly on prednisone. I had this idea in my head I just needed something magical to happen and i'd be able to get off the steroids and things would be ok. Good old denial!
I later met the permanent specialist I have now. Having one person instead of floating means you feel you are building a relationship instead of having to explain your history each time. We discussed things, including the status quo which wasn't ideal.
I'd had other hospitalisations at this point for dehydration. He said I had two real choices drug trials or surgery. I was offered another trial, but it would be a hassle to get to it so I chose to talk to a surgeon without any obligation to have something done.
I found the no obligation bit VERY useful. I ended up talking to them 3 times before I finally agreed to actually go ahead with it. I found they were very patient, and professional as they explained various things about the various options, the procedures, the risks, recovery and life after.
I also spoke to some people I met through a private Facebook group. This was great to hear from real people in the New Zealand system and get an idea what happened. I got to hear the good and bad bits.
Finally, a stoma nurse (bowel specialist nurse) put me in touch with someone who was roughly in the same position. A male with kids. We compared stories and he seemed to be in a much better position now after surgery than before.
The decision to do it
For a long time, I didn't want to do it, partly as it was something I couldn't undo. I was scared, I'd had nothing big like this before. One thing in my favour, I was a father of two toddlers, so I'd had exposure to changing nappies. I got to a point where I was happy enough to go through with surgery, losing part of my bowel and getting a stoma, but I wasn't fully comfortable with it. I really feel for those who have emergency surgery, they have no time to prepare for it, or choice.
SURGERY #1
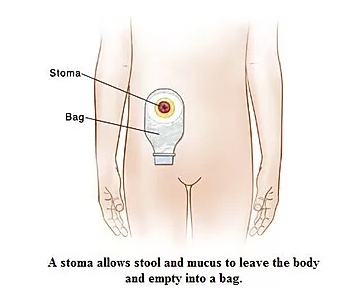
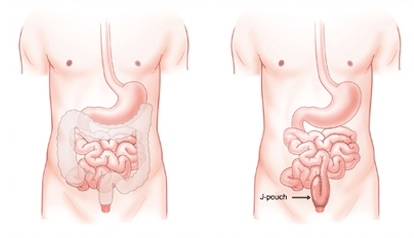
The procedure was to do keyhole surgery, remove most of my bowel and appendix. Get the end of my small bowel and make an end ileostomy. (This is where they remove the whole of the colon through an incision in your abdomen. The end of the small intestine (ileum) is divided and brought out of the abdomen through a smaller incision and stitched on to the skin to form a stoma) . The last 20cm or so of my colon was stapled up and just left internally.
The procedure went well, recovery went fairly well. I got home on my 6th day. It took me a day or two before I could make myself look at my stoma. I wasn't allowed to go home until I could both empty my bag, and also change it. The stoma nurses are great here in Wellington.
Getting over major surgery is a big thing and it takes time, but everything went well. After about two home visits with the stoma nurse, I had the hang of it.
Pretty much all my old symptoms and problems were gone. I did have a few new things to deal with, but the big thing was I could just get on with my life. This cannot be understated. I didn't have to worry about being late to things, or having to rush out to get to the toilet.
I also did not require my medication anymore! I pretty much did everything as normal.
SURGERY #2
After about 13 months I went for the 2nd surgery. Most of this delay was due to me building up enough leave from work to cover for my time I would need to recover, otherwise, I could have done it earlier.
This procedure was to remove the last bit of colon, and pull my small bowel down and create a "Pouch" from it to collect the waste internally and connect to my rectum so I have the ability to go to the toilet again and not through a bag on my side. I still have to keep my stoma at this stage until it is healed enough and prove there are no leaks internally. Then I'll take the stoma away and have function again, (3rd surgery).
A lot of things did not go well this time.
1) My scheduled day anaesthetists were sick. After 5 hours of waiting for someone else to turn up, I was sent home. I went to work for 4 days and got my surgery the following week.
2) I'd put on weight since the last surgery, so keyhole surgery wouldn't work now. I got cut open this time, it wasn't as straight forward as it should have been, but they managed to connect things up. I was also told there was a lot of scar tissue inside, even though on the outside things seemed great.
3) I got a complication called ileus. My bowel went to sleep for 6 days. What this means is any fluids I drank sat in my stomach for a few hours, then violently vomited them up. I had to get a Nasogastric tube put down my nose and the back of my throat to get rid of everything.
4) When the ileus finally woke up, my output from the stoma was incredibly watery. I needed up to 8 loperamide a day (treatment for diarrhoea) as well as codeine to try to combat this.
5) When they went to remove my staples, my wound opened up again.
6) My wound got infected which meant extra pain and pills.
7) The size/shape and everything about my stoma were not ideal compared to the first one. The first time I was lucky, I could just get a bag, put it on and that was it! No leaks. This time I had to measure and cut an odd shape (the stoma kept changing over time). I had to get seals to try to stop leaks. I had to wear a belt to hold it in place.
8) Unlike the first time, over time poo would seep out. This burns your skin (it's acidic bile), you need to change the bag more often, and the risk of leaking poo wherever you go is not ideal. Sometimes I got the shape of the stoma hole wrong for the bag and did 3 bag changes in a few hours. Very demoralising.
9) I've had an area of skin which has been red, raw and right next to the stoma. Its been very hard to let it heal as output from the stoma would get onto it and make it worse.
Things have though, improved with time.
I need less medication now than pre-surgery. I get less pain now, but I'm always checking for issues.
SURGERY #3 (The future)
I haven't had this yet, but the next bit is to join up the 2 ends of my loop ileostomy, close up the stoma hole and then I can use my new pouch. I currently have 2 obstacles stopping me from requesting this.
1) No leave at work
2) I've been told that while this is normally quite a minor procedure, there is a chance I might need to be cut open again. This would mean a long 6-week recovery. It means I could get complications like an ileus or other again. This makes me very nervous.
For a planned surgery like this, it's important to talk to those who will be affected in your life. I worked out a plan for my family, mostly how they could cope when I was incapacitated and my recovery. I also had to plan with work for being away for several weeks, then when I could do some work from home, it took time before I could do a full days work. (Check out your ACC options).
Overall though, I'd never choose to go back to my diseased bowel, even compared to the bad days I have now.