Ulcerative colitis, otherwise known as Colitis, UC or Ulcerosa is one of the two major types of inflammatory bowel disease (IBD), the other being Crohn's Disease. Both Crohn’s Disease and Ulcerative Colitis are believed to be autoimmune diseases, where the body reacts against its own tissues.
IBD affects over 28,000 people in New Zealand and is growing.
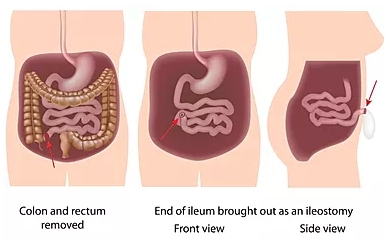
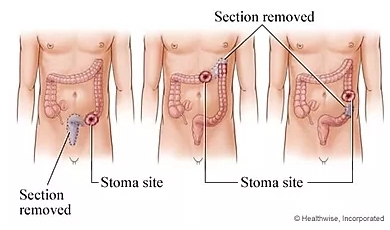
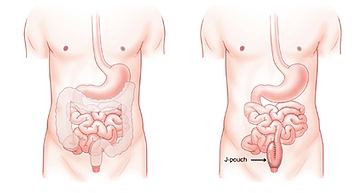
The main difference between the two conditions is that, Crohn’s Disease can affect any part of the digestive tract, Ulcerative Colitis affects only the large bowel and the rectum.
While Crohn’s Disease can affect all layers of the bowel wall, Ulcerative Colitis only affects the lining of the colon.
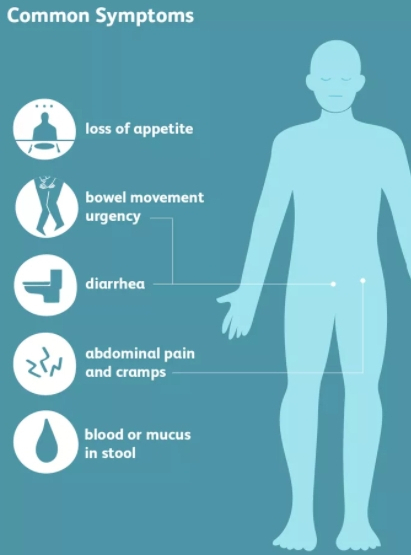
Ulcerative Colitis causes inflammation of the cells that line the rectum and colon (large intestine / large bowel). This inflammation can lead to sores called ulcers which may bleed and interfere wth digestion.
The immune system mistakes food, bacteria, and other materials in the intestine for foreign or invading substances. When this happens, the body sends white blood cells into the lining of the intestines, where they produce chronic inflammation and ulcerations.
Colitis can mimic the symptoms of bowel cancer and some reports suggest up to 15% of IBD patients go on to develop bowel cancer later in life.
Have a look at this quick 4-minute video explaining Ulcerative Colitis...